The Counterpoint is a free newsletter that uses both analytic and holistic thinking to examine the wider world. My goal is that you find it ‘worth reading’ rather than it necessarily ‘being right.’ Expect regular updates on the SARS-CoV-2 pandemic as well as essays on a variety of topics. I appreciate any and all sharing or subscriptions.
The hyper-infectious Delta variant of SARS-CoV-2 continues to spread within the United States. In less than one month, we’ve moved from ‘record low case counts’ to ‘second-largest wave of cases’ yet. The United States is back above 100,000 cases per day (below).
The Delta variant present a significant and concerning increase in evolutionary fitness for SARS-CoV-2. It is truly hyper-infectious, displays a certain amount of immune-evasion, and the evidence suggests that it causes more significant disease across more age ranges.
As much as we all wanted the pandemic to over; it’s not. Premature rollback of public health measures combined with inadequate vaccination levels left the United States vulnerable. The Delta variant exploited that vulnerability.
The current situation is complex and defies easy explanation. It is neither doomsday nor back-to-normal. Some good, bad, and ugly caveats are explored below.
The Good
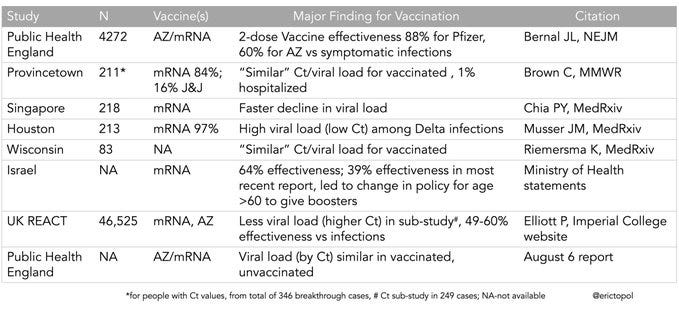
All authorized vaccines continue to provide robust protection from serious disease and death due to COVID-19. A summary of vaccinations with respect to the Delta variant is provided below, credit to Dr. Eric Topol.
The totality of this data suggests that the effectiveness of the vaccines has been significantly reduced, from ~95% to ~60%. But a reminder that vaccine effectiveness is measured in terms of infection. If you’re vaccinated, it’s fairly likely that you will be infected and, if infected, you can have a similar viral load as an unvaccinated person. But because the vaccine trained your immune system to recognize the virus, it is extremely unlikely that you’ll be hospitalized and/or die. The CDC tracks severe “breakthrough cases” and so far, out of ~165 million vaccinated Americans, only 5,285 have been hospitalized for COVID-19 (0.003%) and 1,191 have died (0.0007%).
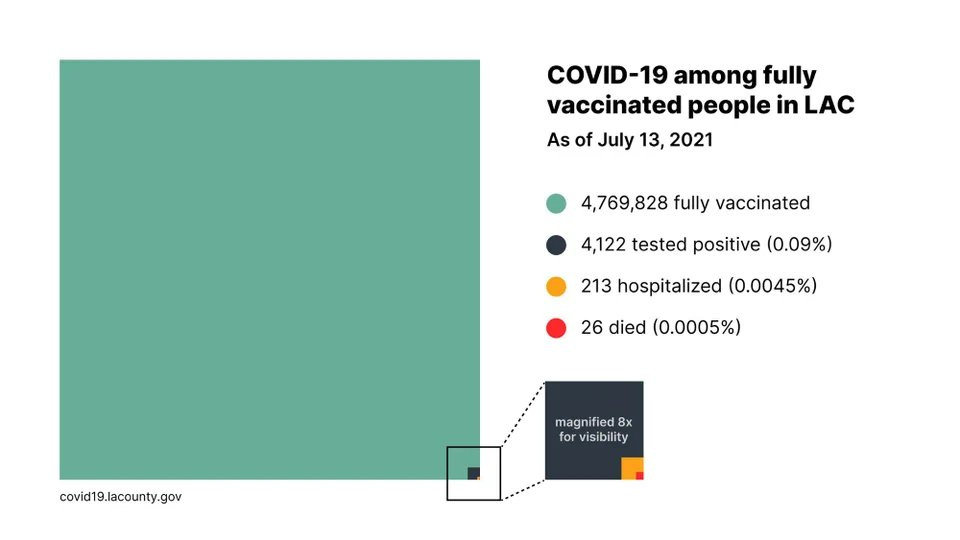
Number can be abstract, so below is a visual representation of Los Angeles County’s data, credit to Garrett Watson. Note, this data is a few weeks old and as Delta continues to spread, more and more breakthrough infections have occurred (the dark blue), but breakthrough hospitalizations and deaths remain extremely low.
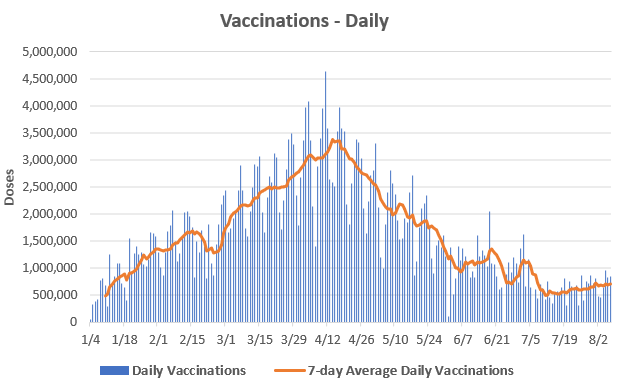
Finally, the Delta wave is convincing people to take the vaccine. The seven-day average of daily vaccinations have increased from ~488,000 on July 11th to ~712,000 on August 7th (below). It’s unfortunate that it took a fifth wave of cases and the increase is only modest, but we should celebrate any and all increases in vaccination rates. The vaccines remain our strongest tool against COVID-19, especially when combined with masks and ventilation.
The Bad
The main problem within the United States continues to be an astounding level of vaccine hesitancy. Despite being monetarily free, widely available, and overwhelmingly effective, the United States remains less vaccinated than essentially every other first world nation.
There are many reasons for vaccine hesitancy. For example, the vaccines are (bafflingly) still not fully approved in the United States, despite surveys showing that full approval is one reason for not seeking vaccination yet. This is something that will hopefully be corrected soon.
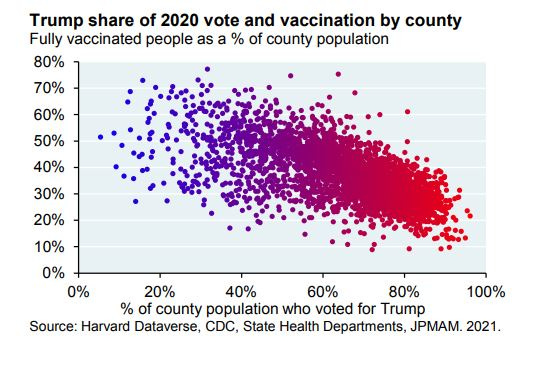
Unfortunately, the vaccines and public health in general, were politicized, and this is something that seemingly won’t be corrected anytime soon, if ever.
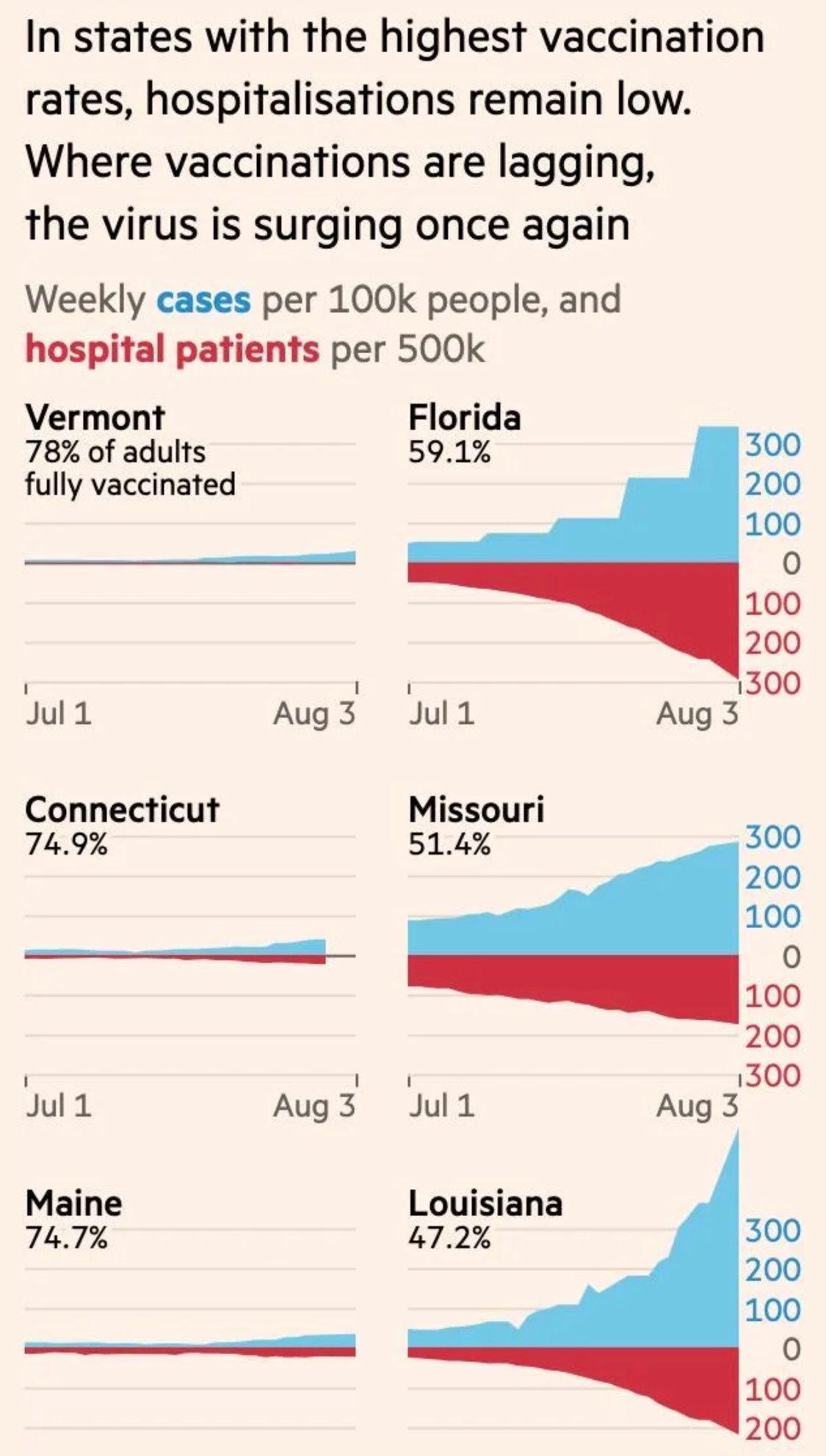
It’s hard to reconcile the only modest increases in vaccinations despite hospitalizations surging in low-vaccinated communities (below). If hospitals being overwhelmed in summer 2021 will not convince individuals to be vaccinated, it’s likely that they never will.
Let’s be clear about the situation: while the pandemic is primarily affecting the unvaccinated, the situation affects us all.
“Our ICU capacity is reaching a critical point where the level of risk to the entire community has significantly increased, and not just to those who are needing treatment for COVID. If we fail to come together as a community now, we jeopardize the lives of loved ones who might need critical care.” Dr. Desmar Walkes of Austin-Travis County Health Authority.
Hospitals in Texas, Arkansas, Missouri, Alabama, Florida, and many other places are back to critical shortages of beds, staff, and supplies. Watch below as a doctor in Louisiana explains the situation in her hospital.

The worse reality is that there are tens of millions of Americans that are ineligible to receive vaccination, even if they want one. For example, the vaccines are still not authorized for children. Because adults refuse to be vaccinated and refuse to wear masks, hospitalizations for children are at all-time highs.
The Ugly
The reality of the situation is that SARS-CoV-2 is now the latest endemic human coronavirus. Whether you are vaccinated or not, at some point, you will be infected. Of course, one’s vaccination status will heavily influence the outcome of that infection, but there is no more avoiding infection. SARS-CoV-2 is simply too prevalent and too infectious. Where the ancestral strains had R0s of ~3, it’s likely that Delta has an R0 of ~6.
What this means in practice is that without both high vaccination rates and strong public health measures (masks, ventilation, physical distancing, etc), there is no controlling Delta’s spread. Notice that these estimates assume 70% of the population is fully vaccinated ( zero states have achieved this) and 99% efficiency against transmission, which given the high viral loads in some vaccinated individuals, appears to be no longer true. Below image credit to Gosia Gaspero.
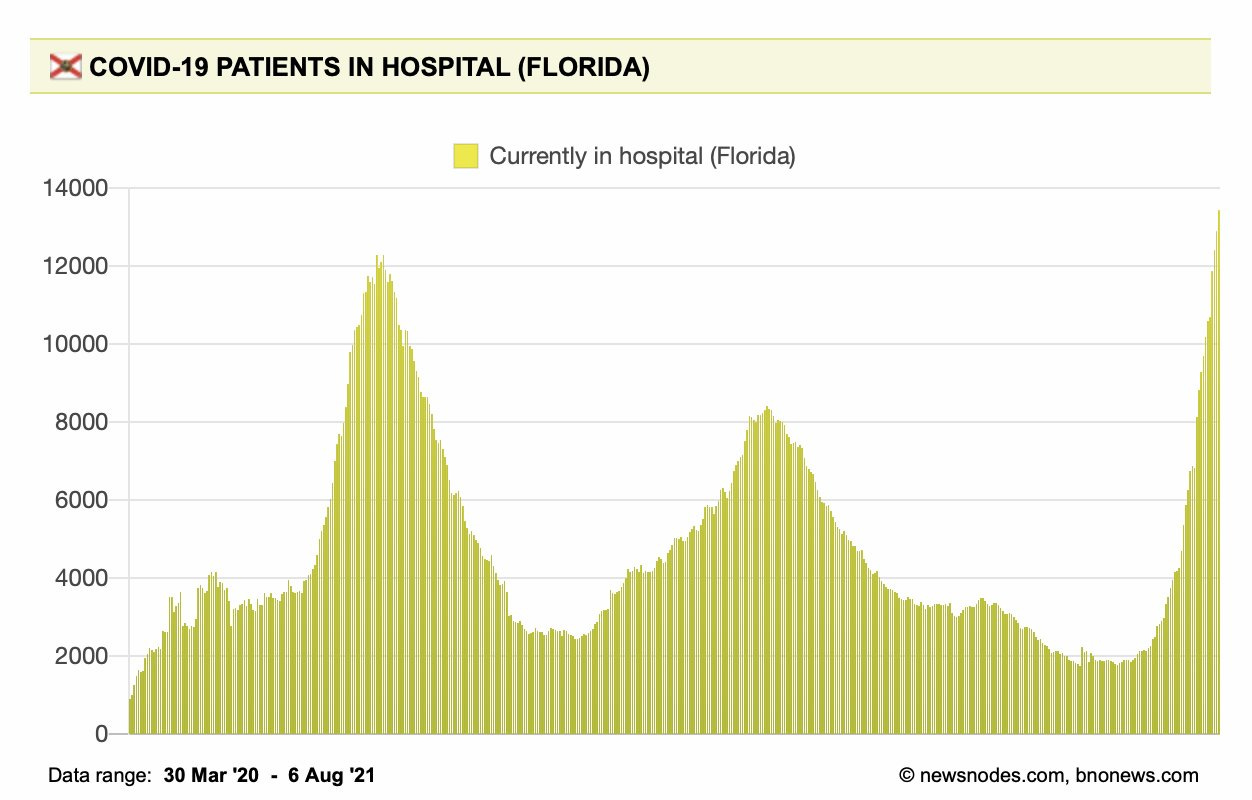
To use a real-life example, let’s look at Florida. With 59.4% of Floridians with at least one dose of vaccine, Florida has an above average vaccination rate. But on the public health front, Florida remains hostile to even basic measures such as indoor masks. Consequently, COVID-19 hospitalizations just surpassed their previous all-time high.
And Florida is just one example. New York has 64.1% of its population with at least one dose, they are much less hostile to public health measures, and keep in mind it’s August, which should be the annual low point of respiratory virus transmission, due to seasonality effects. Despite this, hospitalizations are increasing for every age group in New York state (below), though to a lesser degree than the previously mentioned Southern states. What happens this fall and winter with temperature and humidity that actively promotes viral transmission?
It is likely that without 80+% of the population being fully vaccinated and strong public health measures until next spring, Delta SARS-CoV-2 will continue to spread. Assume that you will be infected. The outcome of that infection will depend mainly on your vaccination status as well as your age and co-morbidity status. Masks and ventilation remain key ways communities can limit viral spread.