SARS-CoV-2: The Final Update (of the Pandemic)
An update and some reflections while we are at the end-of-the-end of the pandemic. Plans for how this newsletter will change as the endemic begins.
The Counterpoint is a free newsletter that uses both analytic and holistic thinking to examine the wider world. My goal is that you find it ‘worth reading’ rather than it necessarily ‘being right.’ Expect regular updates on the SARS-CoV-2 pandemic as well as essays on a variety of topics. I appreciate any and all sharing or subscriptions.
Two Years Later: the End
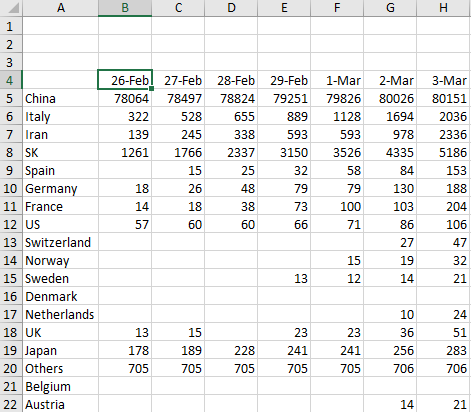
On February 26, 2020, I opened an Excel document and began entering data on SARS-CoV-2's spread. I had been loosely following the virus for perhaps a week or two, but by then it was clear to me that this virus was 'the big one.'
I knew of the eventuality of another respiratory virus pandemic because from 2011-2015 I worked as an undergraduate laboratory assistant in the Nutritional Immunology and Molecular Medicine Laboratory at Virginia Tech. Our lab studied the underlying inflammatory mechanisms of multiple autoimmune and infectious diseases, including influenza. Specifically, we studied the strain “A/California/07/2009(H1N1)”, more commonly known as the virus that caused the 2009 “swine flu” pandemic. By no means did I become an “expert,” but I did learn many things about influenza, its spread, and its biology.
When California's first stay-at-home order went into effect on March 19th, 2020 , my hours were reduced to two days per week. This newsletter began as a way to keep busy while my wife worked from home Monday through Friday.
After two years, I feel comfortable saying we are in the final days of the pandemic. There are no black-and-white endings with pandemics but it is clear that we are close. This is because:
The Omicron wave was massive, likely infecting over 50% of the population. This will establish a broad and deep ‘immunity wall’ for the next several months while antibody levels remain elevated from recent infection.
64.9% of Americans are fully vaccinated. This number is embarrassingly low when compared to other nations. However, it still means that roughly two-thirds of the country has had at least two doses of a safe and highly-effective vaccine, adding to the ‘immunity wall.’
As we move into spring in the North Hemisphere, seasonality effects will begin to suppress viral spread. Seasonality is complex and its causes not fully understood, but the pattern is clear.

The End but not the End
This does not mean SARS-CoV-2 will cease to exist. It is now one of ~200 endemic respiratory viruses. It will continue to cause disease for the rest of our lives.1
While the spring is likely to be mild, the next front to monitor will be cases and deaths in the American Sun Belt during the summer. Large waves of SARS-CoV-2 occurred there during both 2020 and 2021. This is believed to be because the very hot and very humid summers create conditions that functionally resemble winter.2
Though the region has been incredibly hard hit (six of the top ten states with the highest deaths per capita are in the Sun Belt), it also contains some of the least vaccinated states. Thus the level of cases and deaths there this summer will provide insight into both the persistence of natural immunity and the medium-term dynamics of endemicity.
Ideally, cases will remain low throughout the summer but there is significant probability that we will have annual winter waves. It is likely that vulnerable populations (and those that interact with them) will need annual boosters.
Our best route for controlling future respiratory disease is societal-level infrastructure upgrades that do not place the public health burden on the individual. As outlined previously, these should include:
Investment by local, state, and federal governments to increase ventilation and sanitization of indoor air in all public buildings.
Direct investment or tax credit/rebate for individual households to increase ventilation and sanitization of indoor air in private residences.
Updating and setting modern air quality standards, both indoor and outdoor.
Investment and empowerment of internal government agencies involved in pandemic detection and prevention.
Investment in local and state public health departments so that testing capacity, both the collection and processing of samples, can be maintained indefinitely.
Education and outreach campaigns, both targeted and broad-based, by local and state public health departments about the importance of vaccines and staying home when ill.
Mandatory sick leave policy for all workers, regardless of hourly or salary.
Through these and other measures, our generation can tackle airborne diseases, just as prior generations tackled food- and water-borne diseases. We have the ability to exponentially decrease the burden from all respiratory illness. The only thing that is stopping us is ourselves.
The Present
Cases within the United States continue their rapid decline. The Omicron case curve is something that will be studied in all future epidemiology class. The seven-day average of cases is 68,422, a >90% decrease since the peak of ~803,000 on Jan 16th.
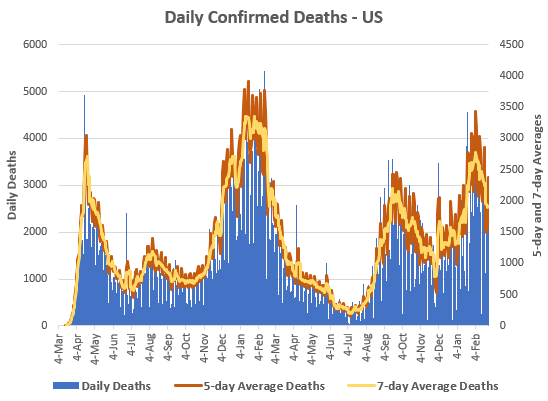
Despite the decline in cases, deaths remain elevated. As we’ve discussed previously, deaths lag cases by a few weeks. The seven-day average of deaths is at 1,907. This is just below the peak of the Delta wave. It will likely take several weeks to return to the lows of July 2021, only ~200 deaths per day. Hopefully, the decline will continue into sub-100 deaths per day sometime this spring.
In total, ~170,000 Americans have died during the Omicron wave. Bring the total to 948,215 confirmed COVID-19 since March 2020. The true toll is certainly over one million.
Vaccinations near all-time lows. The seven-day average for daily vaccinations is a mere 372,000 (below, bottom). This is despite a significant portion of the United States remaining unvaccinated. Only 76.3% of Americans have had one dose and 64.9% have had two doses. Of those that are fully vaccinated, only 43.6% have received a booster dose (below, top).
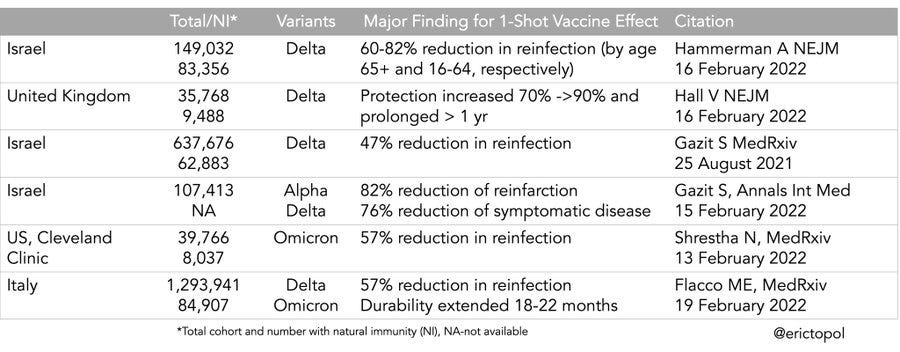
Being fully vaccinated plus a booster is extremely important, especially against Omicron. It is clear that the third dose adds a significant layer of protection from infection. Nine studies summarized below, credit to Dr. Eric Topol.
Even if a breakthrough infection occurs, having the third booster doses exponentially decreases one’s odds of deaths. This is on top of the exponential decrease two doses provides. Below image from the CDC’s COVID-19 tracker.
Prior infection is equivalent to ~1 dose of vaccination. State and local public health authorities should recognize that those with confirmed prior infection do not need three vaccinations. But individuals with only prior infection should recognize that, without supplemental vaccination, they are vulnerable to SARS-CoV-2 reinfection. Summary of six studies showing prior infection + 1-shot vaccination provides high levels of protection. Image credit to Dr. Eric Topol.
Finally, the United States needs to focus on getting the globe vaccinated. While the US has donated more vaccines than any other nation, we need to continue to prioritize global vaccinations. We have over 137,000,000 vaccines in reserve, or 369 days worth at current vaccination rates. The returns, both health-wise and diplomatically, from dosing these vaccines aboard are much higher than letting them expire in US-based freezers. You can follow specifics of US vaccine donations here.
The Future
With the ending of the pandemic, this newsletter will be forced to change. SARS-CoV-2 coverage will continue. In the short term, I have a few pandemic-related newsletters planned. In the medium term, there will be significantly more time between COVID-specific updates.
Moreover, the topics of this newsletter will broaden. I’ve greatly enjoyed regular writing and will continue to regularly produce content. Expect topics to include chemistry and philosophy (the subjects I studied at Virginia Tech), biomedical research (what I do professionally), agriculture (my main hobby) and book reviews.
Thank you
As I stated in the beginning, this newsletter started as a way to keep busy during the initial ‘lockdowns.’ Since then, it has grown beyond the initial family and friends that first subscribed. I hope everyone has found it as informative as I’ve tried to make it.
This newsletter has been incredibly educational for myself. The global scientific and medical response to the pandemic was unprecedented. I’ve never ingrained myself into scientific literature like I have for COVID-19. Sure, I read plenty of papers for my job as a R&D scientist, but it simply doesn’t compare. Both the breadth and depth scientific, medical, and public health research that has been produced over the past two years is something that I remain in awe of, in the most literal sense.
To my subscribers, I hope I’ve proven that I know a thing or two (or perhaps even three) over the last two years and that you remain subscribed as SARS-CoV-2 coverage declines and I broaden into other topics. Again, my aim is to be ‘worth reading’ not necessarily ‘being right.’
You might’ve noticed that the 2009 pandemic influenza was an H1N1, the same family as the 1918 pandemic influenza. This is because the 2009 virus is a direct descendant of the 1918 virus. You can read about the full ‘family tree’ of the 1918 influenza in this NEJM paper, co-authored by none other than Dr. Anthony Fauci. The descendants of both the 1918 and 2009 viruses continue to circulate.
I.e. most people spend most of the time indoors and air-conditioning produces air temperature and humidity that better promotes viral spread.