SARS-CoV-2 Update for June 9th
Omicron BA.4 and BA.5 will likely cause an eighth wave in the United States but immunity remains robust. One's individual risk varies. Risk reduction means "ventilate, vaccinate, high-quality masks."
The Counterpoint is a free newsletter that uses both analytic and holistic thinking to examine the wider world. My goal is that you find it ‘worth reading’ rather than it necessarily ‘being right.’ Expect regular updates on the SARS-CoV-2 pandemic as well as essays on a variety of topics. I appreciate any and all sharing or subscriptions.
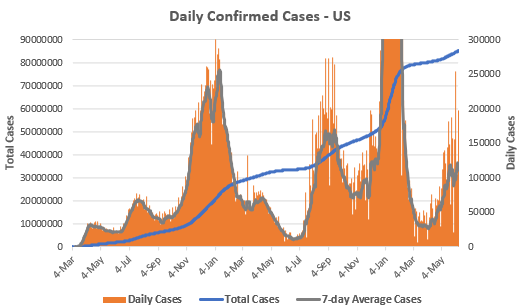
Daily confirmed cases in the United States remain above 100,000, with the seven-day average at 110,778. Memorial Day weekend impacted data reporting, but we are just below the current peak of the seventh wave, which was 121,973 on June 6th.
The true level of infection is certainly far higher. This has been an issue throughout the pandemic because of inadequate testing and asymptomatic illness, but current undercounts have been magnified during both Omicron waves with the availability of at-home rapid tests. A recent pre-print from Dr. Denis Nash, epidemiologist at CUNY, estimates that true infections in New York City were ~30x confirmed case counts.1
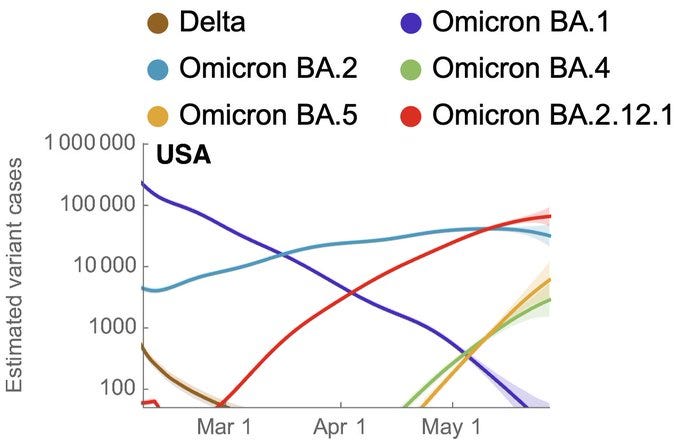
As we’ve reviewed in previous updates, the Omicron strain BA.2.12.1 is currently the main driver of cases in the United States. The CDC’s variant tracker estimates that 62.2% of current infections are BA.2.12.1.
However, Omicron strains BA.4 and BA.5 are growing exponentially and actively displacing both BA.2 and BA.2.12.1. Given the set of mutations in BA.4 and BA.5 (specifically L452R and F486V) it is highly likely that their increased fitness is due to immune evasion, i.e. the capacity to reinfect those with BA.1 immunity (from infection), wild-type immunity (from vaccination), or both (vaccinated + breakthrough infection).
I understand the desire for straight and easy answers. Unfortunately, the situation requires a lot of nuance. In short, BA.4 and BA.5 are quite serious viruses, perhaps the most serious of the pandemic. Given their immune evasion, there is a decent probability that you will be infected with them in the medium-term, especially if you live in the Sunbelt, where cases have been concentrated each of the past two summers. However, immunity is not ‘black-and-white’ and immunity from both vaccination and prior infection continues to provide strong protection from severe outcomes.
Omicron BA.4 and BA.5 are quite severe viruses, representing the second iteration of ‘training’ against the human immune system. The numerous mutations they’ve evolved came about in order to evade the human immune system.
A recent pre-print from Dr. Kei Sato, virologist at The University of Tokyo, suggests that BA.4 and BA.5 are more pathogenic that previous Omicron strains. Infected hamsters had a large reduction in body weight (below), lower blood oxygen levels, more viral RNA throughout the lung, and worse histological outcomes.

In humans, it is clear that BA.4 and BA.5 have significant capacity to evade our antibody response. In a pre-print from Dr. David Ho, virologist at Columbia University, they find a significant drop in neutralization against BA.4 and BA.5 in boosted, non-Omicron breakthrough-infected, and Omicron BA.1 breakthrough-infected patients.
These results were replicated in a study published in Science Immunology from BioNTech and Pfizer looking at viral neutralization against different strains of CoV-2 and the original CoV-1. They divided patients based on both their vaccination and prior-infection status (below, left to right is 2x Pfizer, 3x Pfizer, 2x Pfizer + Omicron infection, 3x Pfizer + Omicron infection, different CoV-2 variants are left-to-right and CoV-1 is the far right in each panel). Double-vaccinated patients had the worst neutralization; triple-vaccinated + breakthrough-infected had the best.
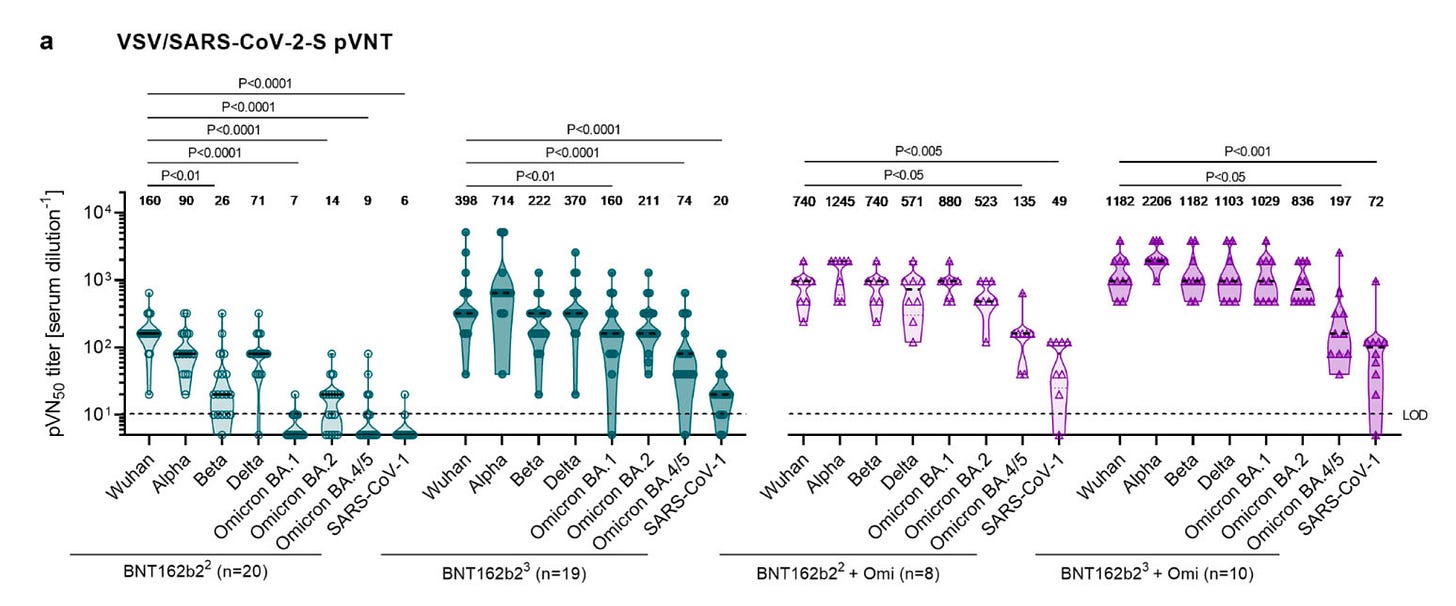
Both these studies suggest that while there is a significant reduction in neutralization, if both boosted and breakthrough-infected, there is some cross-reaction. The best neutralization occurs in both boosted and breakthrough-infected (above, far-right panel), where despite a ~10x reduction in neutralization, it’s still well above zero. This is likely because the combination of wild-type exposure (via vaccination) and Omicron exposure (via breakthrough infection) induces a broad adaptive immune response.
Remember that our immune system is redundant and has multiple layers of protection. Antibodies are important because they can protect you from infection. All things equal, it would be better to have high levels of neutralizing antibodies. But the most important layer for protection from severe disease is our adaptive immune system, specifically our T cells. All available evidence suggests that both vaccination and prior infection induce a robust and lasting T cell response.
Now, I could throw a bunch of ‘science’ at you to support this statement2 but let’s look at real-world outcomes.
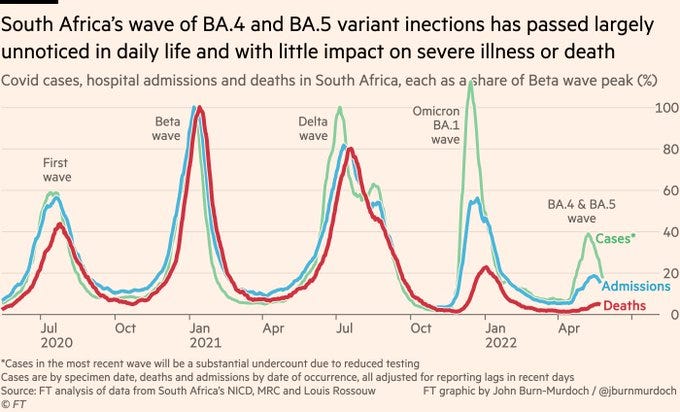
South Africa just experienced a large BA.4 and BA.5 wave. Despite less than half of the population being fully vaccinated, both hospital admissions and deaths were the lowest of any wave yet.
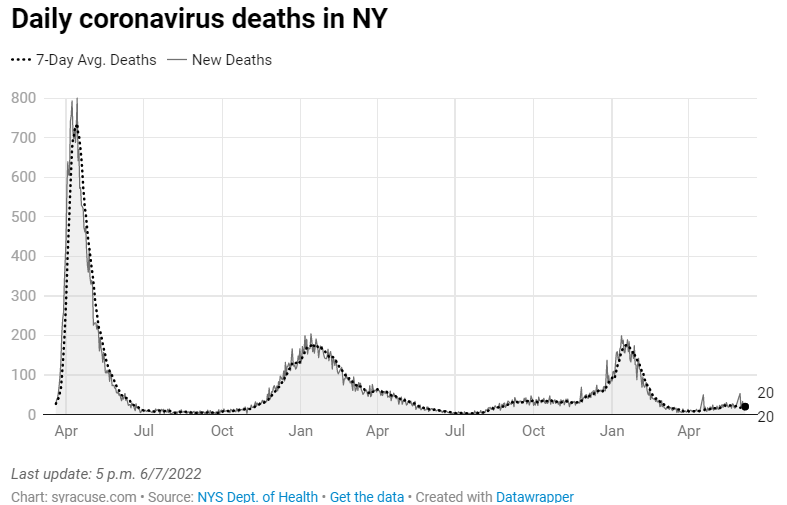
New York State just experienced a large BA.2 and BA.2.12.1 wave. With 77.3% of the population fully vaccinated, hospitalizations and deaths were the lowest of any wave yet.
Notice that the FT graphic caveats cases with “the most recent wave will be a substantial undercount due to reduced testing.” This newsletter began with an epidemiological pre-print suggesting that NYC cases were undercounted.
If the latest waves were substantial undercounts of cases but produced the smallest number of deaths yet, then this only bolsters how much the average fatality rate has dropped despite both more transmissible/more virulent strains of Omicron. This is because both immunity-from-infection (e.g. South Africa) and immunity-from-vaccination (e.g. New York) remains robust and long-lasting.
Globally, deaths from COVID-19 are at their lowest since March 2020. Within the United States, April and May 2022 were the lowest monthly death tolls other than June and July 2021, right before the Delta wave. June 2022 is on track to be only slightly deadlier than May 2022, despite a large wave of BA.2.12.1 and a growing wave of BA.4 and BA.5.
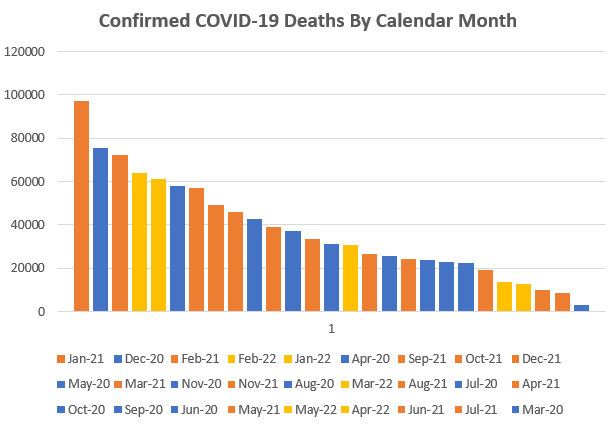
Now, is this death toll “acceptable?” Absolutely not. Annualizing May 2022’s death toll means ~161,000 annual COVID-19 deaths. That is an unreasonable burden to place on our healthcare system and at-risk populations. We need to do better.
Sustainable and long-term solutions include:
Ventilation/sanitization upgrades for all public buildings.
Vaccination campaigns with regularly-updated vaccines.
A culture of voluntary mask-usage during a locality’s ‘cold & flu’ season or whenever cases are elevated.
Robust testing infrastructure so that clusters of cases can be quickly identified.
Increased manufacturing, distribution, and access to COVID-19 therapeutics such as Paxlovid, Evusheld, Bebtelovimab, and Fluvoxamine.
National paid sick leave.
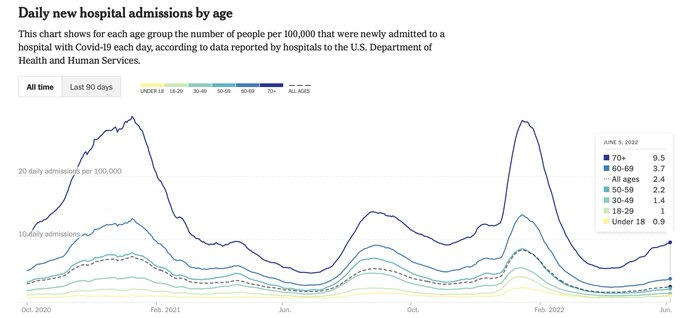
When I say that immunity remains robust, I mean at the population level. Your individual risk is a function of many factors but mainly age, co-morbidity status, and vaccination status. Below is a graph of per capita COVID-19 hospitalization by age. Over 80% of COVID-19 hospitalizations are occurring in those over the age of 50. Over 50% are in those over the age of 70.
Since one cannot change their age and cannot (easily) change their co-morbidity status, the single best thing one can do to protect themselves and others is to remain up-to-date on all vaccinations. A fourth vaccination/second booster is highly effective at preventing both infection and severe disease and is now authorized for everyone over the age of 50 and any immunocompromised person over the age of 12.
Individual risk-reduction continues to mean “ventilate, vaccinate, high-quality mask usage.”
This means would mean that ~22% of NYC was infected in the Omicron BA.2/BA.2.12.1 wave. I don’t know what to think about this study’s exact numbers. True infections are certainly higher but ~30x higher would mean a huge wave, which would have major implications for how we think about CoV-2 (more on this later). Generally, I’d take the ~30x higher with a grain of salt and consider it more of the upper bound of my confidence interval, i.e. the true level of infections lies somewhere between confirmed case counts and ~30x confirmed case counts.
If you do want the science see either this study in Lancet Microbe, this study in Nature Microbiology, this review in Nature Immunology, or this announcement from South Africa’s largest health insurer.