SARS-CoV-2 Update: Omicron
Few, if any, answers but hopefully a framework to think about the newest variant and future ones.
The Counterpoint is a free newsletter that uses both analytic and holistic thinking to examine the wider world. My goal is that you find it ‘worth reading’ rather than it necessarily ‘being right.’ Expect regular updates on the SARS-CoV-2 pandemic as well as essays on a variety of topics. I appreciate any and all sharing or subscriptions.
Because of quick identification by South African scientists (specifically, though not limited to, Tulio de Oliveria) and transparency by the South African government, the global health community is now aware of the latest variant-of-concern, given the name Omicron. We owe a huge debt of gratitude to these researchers and officials.
The quick identification of Omicron means that much remains uncertain. Every and all definitive statements about how this variant behaves should be taken with a massive grain of salt. The transmissibility, immune evasion, and lethality of Omicron all remain unknown. Moving forward, remember that no single study produces truth, no single expert is unbiased. Rigorous scientific endeavor takes time and every day the global health community will move closer to converging on a consensus regarding this variant.
Laboratory Data
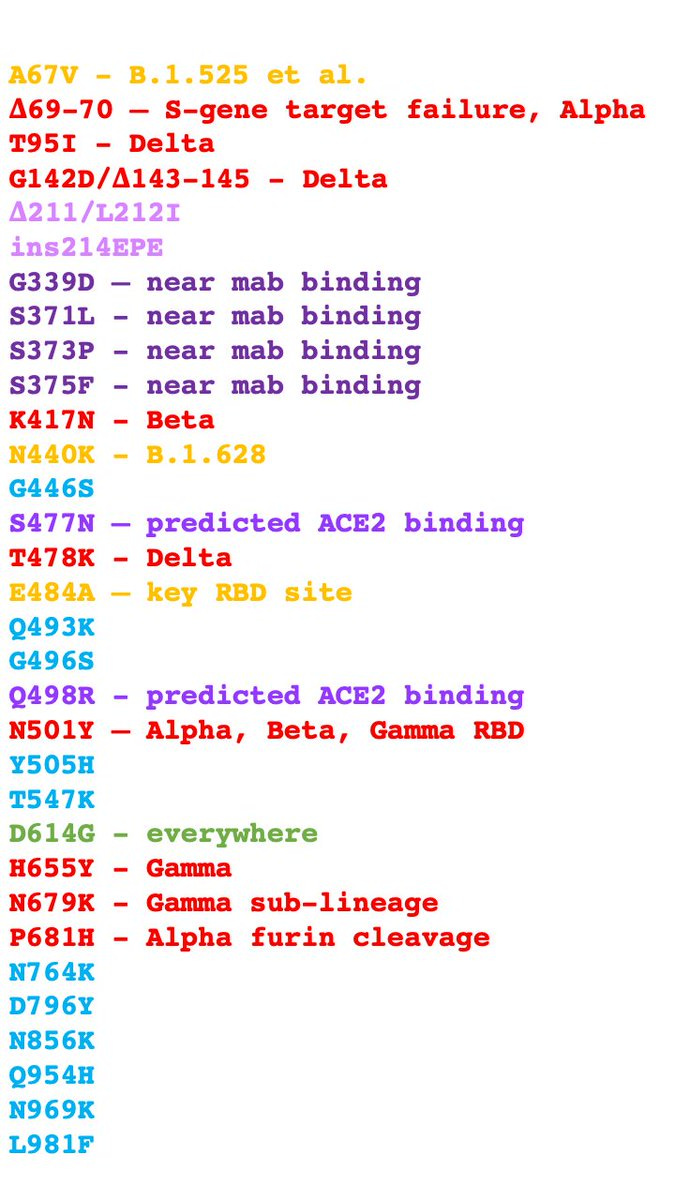
What we do know is that Omicron has an absolute slew of mutations, with 32 mutations in just the spike protein (for comparison Delta has nine in the spike protein). The full list1 is below and color-coded by our current level of knowledge. Credit to Dr. Jeffrey Barrett.
Red: There are nine mutations that we’ve seen in previous variants-of-concern. The specific variants this mutation is present in are listed. Bad.
Purple: New mutations but we have lab data that suggest they are a threat. Probably bad but unknown.
Yellow: New mutations that might mean something because of their location, but we don’t know yet. Unknown.
Blue: Changes never seen before. They may mean something or may mean nothing. We simply don’t know. Unknown.
Green: D614G was not present in the original SARS-CoV-2, but occurred so early in 2020 that it’s essentially part of the ‘wild-type’ virus and has been present on every variant-of-concern. Not concerning.
The red-coded ones definitely concerning since they are present in the other variants, all of which have some level of immune-evasion and/or increased transmissibility. But even excluding these, such a large number of novel/predicted-to-be-bad mutations is concerning. It’s been previously predicted that ~20 mutations in the spike protein are necessary for significant immune-evasion (see this paper in Nature from September 2021). For some good news, mutations don’t always work together additively, i.e. two bad mutations don’t always equal very bad, etc. This is a phenomenon known as epistasis (and a huge reason why we should avoid speculation and wait for concrete studies to be completed).
More than just the number, it’s the breadth of the mutations that are concerning; they are spread over all subunits (areas) of the spike protein, meaning that from every angle, it’s roughly a new shape. And a few of the purple-coded mutations have been previously predicted to dramatically increase binding to the human ACE2 receptor (see this paper in Nature Microbiology from August 2021).
Moreover, many mutations are in areas where the current monoclonal antibodies bind, suggesting that these cocktails may no longer work as well as treatments for COVID-19. This was first suggested last week by the Bloom Lab at the Hutch Institute. This morning, Regeneron announced that preliminary testing with it’s antibodies suggested the prediction of less effectiveness is true.
That is a lot of info to take in but the below slide, from this presentation by the South African health ministry is a nice summary.
In short, Omicron’s set of mutations gives rise to three major concerns.
Increased transmissibility.
Increased immune evasion.
Increased infectivity (severity).
Omicron has the potential for all three. Taking these in order:
Increased transmissibility: The exact R0 remains uncertain. As a reminder, the original strain’s R0 is estimated to be ~3. The Delta variant’s R0 is estimated to be ~6. Nicholas Christakis predicts Omicron’s is in the range of 4-8. Trevor Bedford believes it may be closer to 4. Metaculus, a global prediction market, currently has it at 6.05 (note, this link updates in real time). It remains unknown, but it’s still quite a possibility that Omicron is no more transmissible than Delta, and possibly even less so (though also possibly more so).
Increased immune evasion: Also uncertain. The previously mentioned Trevor Bedford is firmly in the immune evasion camp, and believes that the rapid rise in cases (more on this later) is due to this (the theory being cases are increasing not because Omicron is more transmissible, but because it has more ‘targets’ since it can infect some previously-immune individuals).
Even if Omicron has a moderate level of immune evasion, it wouldn’t be a catastrophe. Studies suggest that vaccines retain effectiveness even when neutralization drops. This is because immunity isn’t black-and-white and Kai Kupferschmidt suggests we switch to the term “immune erosion.”
The human immune system has remarkable redundancies built within it. Even if Omicron can escape the average person’s neutralizing antibodies, they would still have non-neutralizing antibodies, B-cell responses, and multiple types of T-cells that can inhibit or stop the virus. It’s likely that even with significant immune-evasion, both previously infected and/or previously vaccinated individuals would still have better outcomes than an immune-naïve individual.
And, besides for the monoclonal antibody cocktails, the rest of our therapeutics should continue to work against Omicron. Both dexamethasone and remdesivir remain important pharmaceuticals and moving forward, both Merck’s and Pfizer’s new antivirals should be authorized and/or approved extremely soon (then it becomes a manufacturing and distribution challenge, as well as a testing challenge, since both drugs must be given within days of infection).
Finally, both Moderna and Pfizer are working to update their vaccines. The beauty of mRNA vaccine technology is that we can customize the mRNA to code whatever protein we want (in this case, Omicron’s highly-mutated spike protein). Here is Pfizer’s CEO on Twitter today saying they’ll have an updated vaccine in ~100 days:

Increased infectivity (severity): This is the most uncertain and will take the longest to sort out. Early reports suggest less severity but these should be taken with a massive grain of salt. There simply aren’t enough cases yet to determine one’s individual risk given their age, comorbidity status, and vaccination status. Even if South Africa confirms that they are seeing less severity, that doesn’t necessarily translate to other countries. South Africa has a much younger population than first-world nations and variants can attack populations differently (the most famous example of this is the influenza that caused the 1918 pandemic; it killed many people in their 20s, something extremely rare for influenza).
Real World Data
The earliest2 case of Omicron was in Botswana on November 11th. It was detected in South Africa three days later. It’s now been detected in Australia, Belgium, Botswana, Britain, Denmark, Germany, Hong Kong, Israel, Italy, the Netherlands, France, and Canada. In other words, we should assume it’s everywhere.
In South Africa (the ‘leading-edge’), Omicron has increased from 0% of cases to ~75% of cases in about two weeks (below, top), meaning it is out-competing Delta. However, it did so when South Africa had a minimal absolute number of cases (below, bottom). Phrased another way, it would be much more impressive (and terrifying) if Omicron was out-competing a large Delta wave.
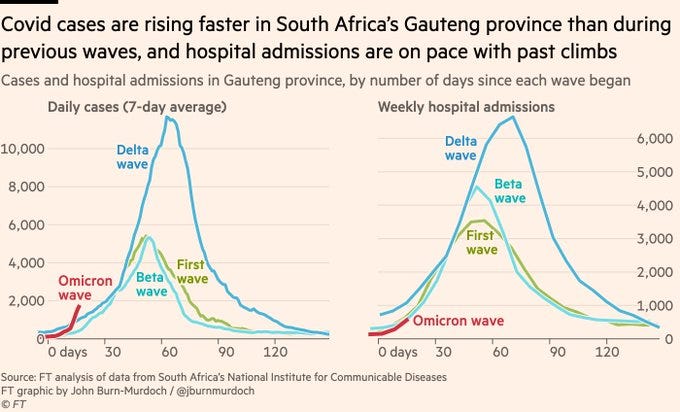
Regardless, a rapid increase in cases is never a good sign. If you compare the rate of increase of cases of the Omicron wave, this wave is rising more rapidly (below). Fortunately, hospitalizations are on pace with previous waves, with the caveat being that South Africa is more vaccinated now than during previous ones. Since vaccines are concentrated on the vulnerable first, you’d expect that to blunt the level of hospitalizations.
The Brass Tax
A new variant of SARS-CoV-2 has evolved a multiple of both known and predicted-to-be bad mutations. It may be more transmissible, it may have some capacity for immune-erosion, and it may lead to more severe disease. Or it may not. Its exact physical characteristics remain unknown. Regardless, it is leading to a new and rapidly-growing wave of cases in South Africa and should be assumed to be present in all countries globally.
All of this should be cause for concern, not chaos. Even in the worst case scenario, we are not defenseless. There are no reasons to believe our immunity will drop to zero. In fact, there are reasons to believe that receiving your booster shot is the best course of action. And even in the nightmare scenario where previous vaccinations are useless (highly unlikely!), both Pfizer and Moderna are working to update their vaccines (just like how the influenza vaccine is updated annually). Finally, in the meantime, we have multiple therapeutics that reduce mortality, and in the near future, two additional therapeutics that should greatly reduce mortality.
The always-great Bob Watcher sums up the situation perfectly below:

Moving Forward
SARS-CoV-2 is endemic. I’ve mentioned this multiple times before but let me be specifically clear about what this means: it is no longer a question of if, but when, each of you will be infected with the virus. Depending on your age, you will probably be infected multiple times throughout your life.
The best way to think about SARS-CoV-2 is influenza.3 Influenza is less transmissible than SARS-CoV-2. Influenza is less lethal than SARS-CoV-2. Influenza has a moderately-effective vaccine that is updated annually and widely available.
Influenza still kills ~35,000 Americans per year.
With SARS-CoV-2 being more transmissible, more lethal, and vaccine uptake continuing to remain a problem in the United States, it’s highly likely that COVID-19 will annually kill >35,000 people. It would not be surprising if it was regularly a top ten cause of death. Annual top ten for last six years shown below (source).
Your outcome with your eventual SARS-CoV-2 infection will depend heavily on three factors: your age, comorbidity status, and vaccination status.
Obviously, we cannot control our age. However, the other two are absolutely within our control.
The vaccines remain widely available and monetarily free. Please schedule your appointment today, regardless if it’s your first, second, or third dose.
Heart disease, diabetes, obesity, and pulmonary disease are the main comorbidities that predict severe outcomes. If you have any of these, or are at risk of developing them, please consult with your physician(s) about possible treatments, including pharmaceuticals, but also nutrition and exercise.
To clarify some of the science jargon: There are twenty amino acids that life builds proteins out of. We use a letter as shorthand for each, e.g. G is glycine, W is tryptophan, etc. When produced proteins are first a 2-D chain than is then folded into a 3-D shape. The first amino acid in the chain is the 1 position, the second the 2 position, etc. In the list of mutations, N501Y means that what should be asparagine (N) at the 501th position is now a tyrosine (Y). The Greek letter delta (the triangle) is used for deletions and the English letters “ins” are used for insertions.
That we know of. It’s unlikely this was truly the first case. Today, reports of Omicron in Europe much earlier than previously known were reported. This would make some sense as it’s been reported that viral evolution mainly occurs in the immunocompromised, not the unvaccinated (see this case report in NEJM from Dec 2020). Immunocompromised individuals tend to live in first-world nations.
Which is deeply ironic because for the longest time, people (including myself) specifically said to not compare it to influenza. This was because, even early in the pandemic, SARS-CoV-2 was clearly deadlier than influenza. However, the long-run infection dynamics of human respiratory viruses spread seasonally via both droplets and aerosols should be roughly the same.